 Vitamin D was traditionally thought of solely as a vitamin required for bone formation and calcium homeostasis. However, the role for vitamin D in human health has widened considerably in the last few decades, and low circulating levels of the vitamin have now been shown to be associated with cardiovascular disease, obesity, insulin resistance, multiple sclerosis, cancer and diabetes. In response to these findings, interest in vitamin D has grown and vitamin D is now being actively and extensively researched. This research and academic interest has had downstream effects on the interest shown by the general public, and as a result many individuals now take vitamin D supplements for their health effects. One of the main problems with vitamin D is that it can be present in the diet and can also be synthesised in the skin by the action of ultraviolet light in the skin. This makes determining the amount of vitamin D required in the diet very difficult as many factors affect the synthetic rate of the vitamin from the sun.
Vitamin D was traditionally thought of solely as a vitamin required for bone formation and calcium homeostasis. However, the role for vitamin D in human health has widened considerably in the last few decades, and low circulating levels of the vitamin have now been shown to be associated with cardiovascular disease, obesity, insulin resistance, multiple sclerosis, cancer and diabetes. In response to these findings, interest in vitamin D has grown and vitamin D is now being actively and extensively researched. This research and academic interest has had downstream effects on the interest shown by the general public, and as a result many individuals now take vitamin D supplements for their health effects. One of the main problems with vitamin D is that it can be present in the diet and can also be synthesised in the skin by the action of ultraviolet light in the skin. This makes determining the amount of vitamin D required in the diet very difficult as many factors affect the synthetic rate of the vitamin from the sun.
The active metabolite of vitamin D in the plasma is 25-hydroxyvitamin D, and it is this metabolite that is measured clinically in order to determine an individual’s vitamin D levels. Blood tests are the best way to measure 25-hydroxyvitamin D concentrations in the blood, and therefore it is not easy for the average person to determine their requirement for vitamin D without medical intervention. Determining a dietary intake is important because unnecessary supplementation can be hazardous due to the toxic nature of vitamin D when plasma levels become excessive. A number of clinical estimates of vitamin D are available that do not require a blood test and these may provide some guidance as to the amount of vitamin D supplementation required to obtain optimal levels in the blood. Some of these involve use of an algometer (these will be covered in another article). However some are based on simple questionnaires and these have been assessed clinically for their ability to accurately predict 25-hydroxyvitamin D levels.
For example in one such study, a group of researchers assessed a vitamin D scoring system against a number of questions that had been obtained from known associations with vitamin D. A score was obtained by adding the values obtained in individual questions and this then was then used to determine the risk of vitamin D insufficiency. The accuracy of the scoring system was then assessed against external validation of the scores through measurements of the subjects blood levels of 25-hydroxyvitamin D. The results of the study showed that questionnaire provided an accurate estimate of the risk of vitamin D deficiency in the subjects tested, with a score of between 7 and 9 being indicative of a moderate risk of vitamin D insufficiency and a score of more than 9 being indicative of a high risk of vitamin D insufficiency. This scoring system may therefore be a useful and quick assessment of the possible risk of vitamin D insufficiency in an individual. The scoring table used in the study is provided below.
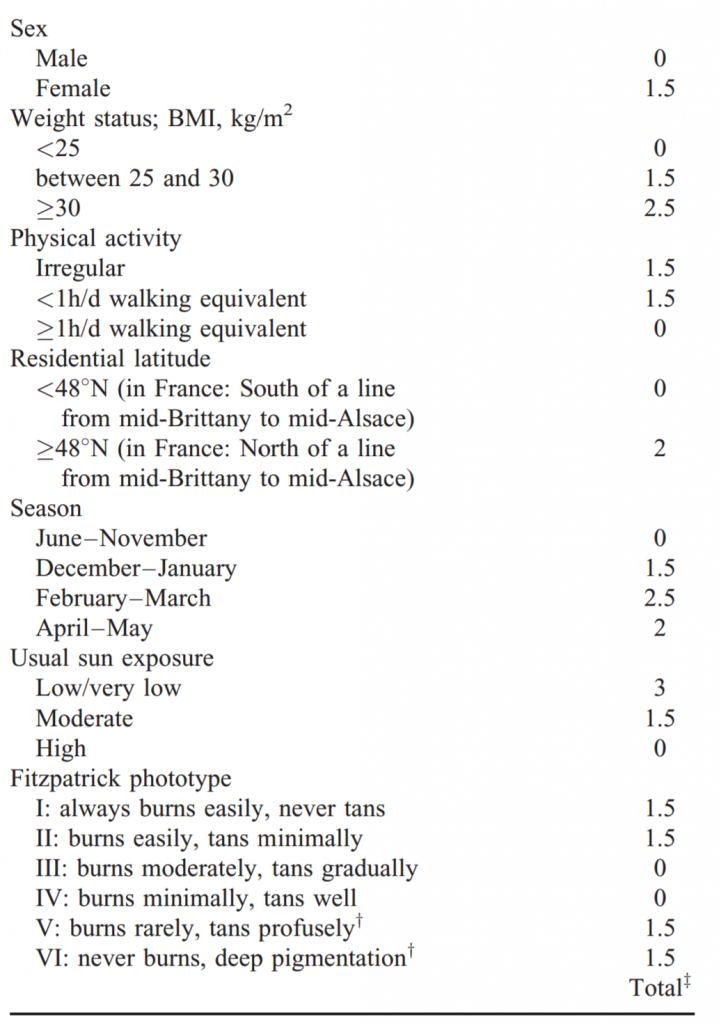
A simple vitamin D scoring system that can accurately estimate the risk of vitamin D insufficiency. A score of less that 7 indicates a low risk of vitamin D insufficiency. A score of between 7 and 9 indicates a moderate risk of vitamin D insufficiency. A score above 9 indicates a high risk of vitamin D insufficiency. BMI = body mass index
Eat Well, Stay Healthy, Protect Yourself
RdB
