Sterols are group of plant compounds with structures similar to the steroid cholesterol (here). Sterols are of interest to nutritional scientists because they show the ability to lower plasma low density lipoprotein (LDL) concentrations. The similarity in structure between the steroid and sterol molecules suggests that their ability to modulate plasma cholesterol concentrations comes from interaction with the same proteins as cholesterol. This has lead to speculation that sterols may effectively inhibit enzymes and act as substrates for transporters that are required for cholesterol metabolism and absorption. The observation that plant sterols lower circulating levels of LDL cholesterol might suggest that sterols are able to prevent the absorption of cholesterol in the gut. The mechanism by which cholesterol is absorbed is not fully understood, but evidence showing decreases in cholesterol absorption with use of inhibitors in a saturable manner is supportive of a protein mediated mechanism.
Candidates for the transporter that might cause absorption of cholesterol include Neimann-Pick C1-like 1 (NPC1L1), scavenger receptor B-1 (SR B-1), and fatty acid translocase (CD36)1. These proteins may transport cholesterol across the apical membrane of enteroctyes to the interior of the cells, where they are repackaged into to chylomicrons with fatty acids, and absorbed from the basolateral membrane to the lymphatic system. The scavenger receptor B-1 is thought to allow cholesterol absorption from the duodenum and jejunum, whereas CD36 is thought to allow cholesterol absorption from the jejunum and ileum. The Neimann-Pick C1-like 1 may act to traffic the cholesterol within the enterocytes. Absorption of cholesterol is regulated by two ATP-cassette binding proteins (ABCG5 and ABCG8) on the apical membrane of the enterocytes, and these proteins efflux intracellular cholesterol back to the lumen of the gut to limit absorption. Effluxed cholesterol may then be excreted in the bile (figure 1). 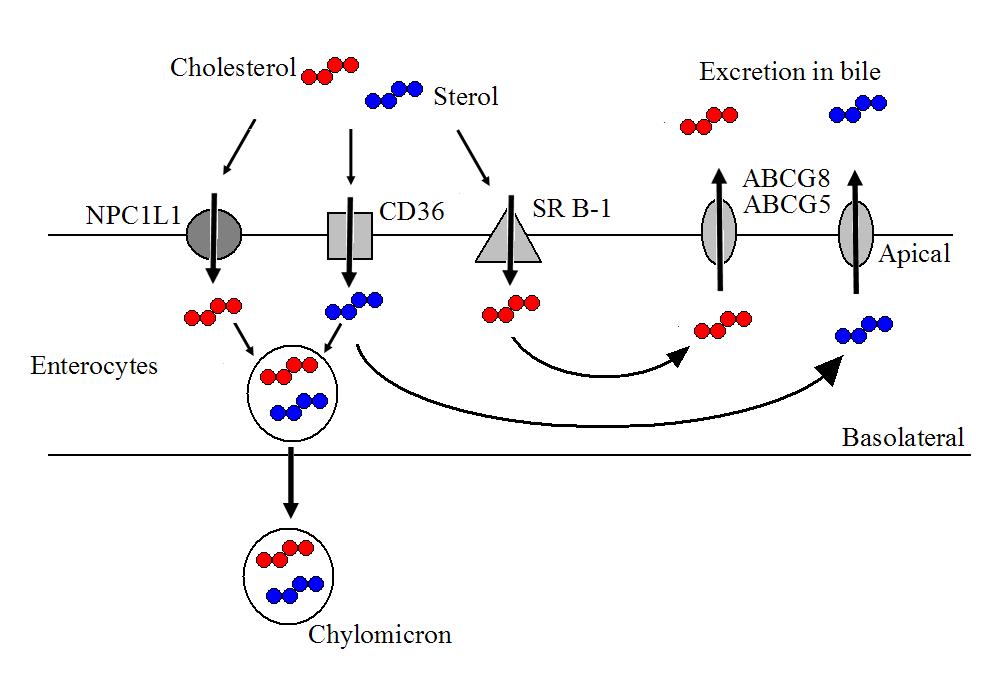 Figure 1. Possible mechanisms of cholesterol and sterol absorption from the human gut. NPC1L1 = Neimann-Pick C1-like 1; SR B-1 = scavenger receptor B-1; CD36 = fatty acid translocase.
Figure 1. Possible mechanisms of cholesterol and sterol absorption from the human gut. NPC1L1 = Neimann-Pick C1-like 1; SR B-1 = scavenger receptor B-1; CD36 = fatty acid translocase.
The intestinal lumen may limit the absorption of sterols using the same intestinal efflux proteins as for cholesterol. The two ATP-cassette binding proteins, ABCG5 and ABCG8 are thought to interact with plant sterols and severely limit their absorption to around 5 % of dietary intakes. Interestingly, individuals with deleterious mutations in the ABCG5 and ABCG8 genes may exhibit massively increased plasma concentrations of plant sterols. Being homozygous recessive for either of these transporters can increase plasma levels of phytosterols 10 to 30 fold (to ~8-60 mg/dL). The increased plasma concentrations of sterols seen in individuals who possess no working copies of either the ABCG5 or ABCG8 protein results in the development of phytosterolaemia (sitosterolemia). However as only one gene is required to code for the transporter, heterozygous individuals appear to exhibit only minimal changes including slight elevations in certain lipoproteins.
High sterol plasma concentrations, as seen in phytosterolaemia, results in the development of atherosclerosis and raises the risk of cardiovascular disease. This is caused by deposition of the sterols in walls of coronary arteries, although disposition occurs in other locations such as skin and tendons. As a result such individuals are recommended to reduce dietary intakes of plant sterols. However, those who are heterozygous for phytosterolaemia might not need to limit sterol intake. Researchers2 have investigated the effects of sterols on plasma lipoprotein concentrations in individuals heterozygous for phytosterolaemia. Using a double-blind randomised controlled trial, 10 subjects with phytosterolaemia and 15 controls consumed 1.6 g/d of phytosterols or a placebo for 4 weeks. Plasma cholesterol concentrations were significantly reduced in both groups (-2.73 and -3.12 mmol/L in phytosterolaemic and healthy individuals, respectively) when compared to a placebo. Both groups also saw increases in plasma campesterol and β-sitosterol concentrations.
This study is interesting, because it also shows that cholesterol absorption was reduced by 22 and 17 % in the phytosterolaemic and healthy individuals, respectively. This suggests that phytosterols do inhibit cholesterol absorption, possibly though interaction with the same intestinal transporters. Just how this effect manifests itself is not know, but may involve inhibition of NPC1L1, SR B-1, and CD36 transporters in the gut. Measuring the cholesterol and sterol concentrations in the bile might have given clues as to this interaction, but this experiment was not performed. In addition to the reduction in absorption of cholesterol, subjects in experienced an increase in endogenous cholesterol production amounting to between just over 20 %. This supports other studies that show that dietary restriction of cholesterol results in little net change due to the hepatic endogenous production of cholesterol maintaining plasma concentrations.
No studies have to date shown a beneficial effect for phytosterols in terms of total mortality. Increasingly, plant sterols are being considered as a viable therapy to accompany statins for cholesterol reduction. However, no one has apparently taken it upon themselves to test the benefit with regard the mortality outcomes of such therapy. Instead the reduction in cholesterol is taken at face value as representing a genuine reduction in cardiovascular risk. That high phytosterol concentrations in phytosterolaemia show the same atherosclerotic symptoms as those with hypercholesterolaemia should be a warning that replacing cholesterol with sterols might not achieve beneficial health outcomes. The use of plant sterols in a pharmaceutical manner has not therefore found to be safe and may indeed be detrimental to health. Cholesterol modulation should therefore occur as a result of an overall high quality diet, rich in soluble fibre from oats and legumes.
RdB
