In recent years it has become apparent that obesity is not a normal physiological response to a positive energy balance as was traditionally believed. Based on evidence in the literature, obesity should now be considered a condition of low-grade chronic inflammation that results from metabolic dysfunction. Obese people are not healthy individuals with excess adipose tissue caused by greed, but have an underlying dysfunction that alters normal metabolism. The result of this abnormality is immune system activation and associated free radical production. Biochemical analysis of abdominal adipose tissue in obese individuals shows that rather than being a simple repository for triglyceride energy, the adipocytes possesses endocrine functions. As adipose tissue accumulates, macrophages invade the tissue, triggering immune responses including the release of cytokines that may contribute to systemic inflammation. This inflammation then causes the generation of free radicals which may initiate the disease process.
For example, C-reactive protein (CRP), a biomarker associated with chronic inflammation, is a strong independent risk factor for cardiovascular disease. Researchers1 have investigated the effects of weight loss on the circulating levels of CRP in 83 otherwise healthy individuals using a very low fat diet. After 12 weeks, subjects lost an average of 7.9 kg body weight and experienced a 26 % reduction is CRP. Correlation statistic showed an association between weight loss and the reduction in CRP, suggesting that weight loss decrease the risk of cardiovascular disease through a reduction in chronic inflammation. Research2 suggests that obese individuals have significantly lower levels of plasma antioxidants that healthy controls. This may result from excessive free radical generation that slowly depletes the plasma reducing power. This may explain the heath benefits of dietary fruits and vegetables that are known to be high in antioxidant nutrients.
If obesity is a condition of systemic inflammation caused by metabolic dysfunction, the question arises as to what is causing the underlying metabolic abnormalities? The answer to this question is not clear, but increasingly low quality diets are being implicated. Low quality diets may cause insulin resistance through dysfunction of the insulin receptor cascade, and this ultimately inhibits the normal cellular uptake of glucose. Fructose is particularly implicated because it increase de novo lipogenesis and raises fasting plasma triglyceride concentrations leading to excessive fat storage in the liver and skeletal muscle. Fat accumulation in these tissues is thought to be the direct cause of the insulin receptor dysfunction, a problem that is magnified by deficiencies of calcium, chromium, vitamin D, and n-3 fatty acids. Low fibre diets may exacerbate the problem due to increases in the speed of glucose absorption that overloads the insulin resistant system (figure 1).
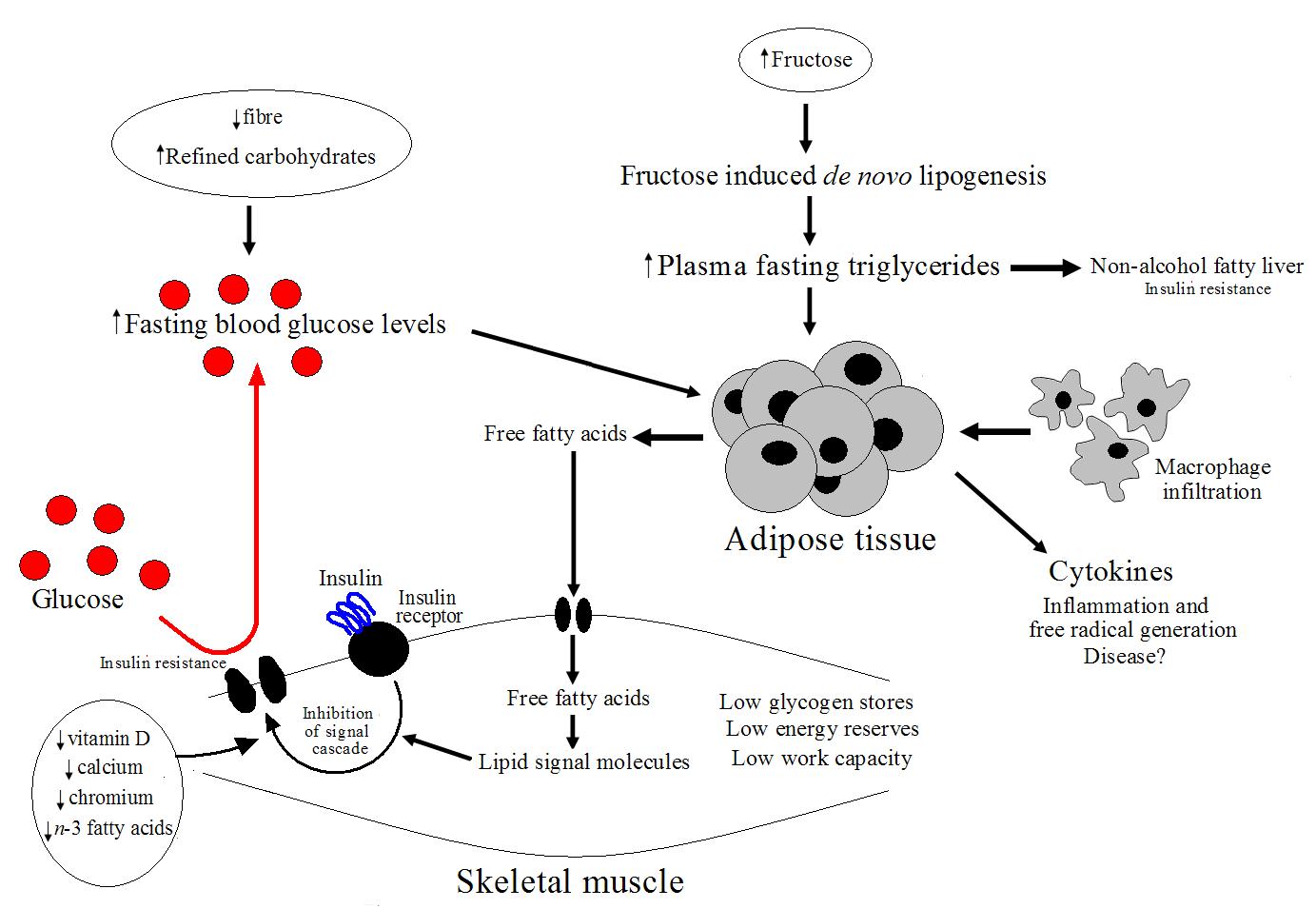 Figure 1. Possible pathway for the development of obesity.
Figure 1. Possible pathway for the development of obesity.
Distancing oneself from the belief that obesity is caused by a simple positive energy imbalance, and considering the possibility that a low quality diet is the route cause of weight gain is a necessary step in understanding weight loss. In the above cited study1 the subjects lost weight through following a traditional energy restrictive diet. It is not uncommon is research to observe such weight loss and most calorie restriction diets are successful initially. However, calorie restriction does treat the underlying metabolic abnormalities and the failure rates of such diets are high for this reason. In contrast, eating a high quality diet, such as the Mediterranean diet, even in the absence of energy restriction has been shown to reduce abdominal adiposity and lower chronic inflammation. The ability of the Mediterraneandiet to reduce systemic inflammation and lower adiposity explains the cardiovascular benefits seen in research.
RdB
